Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

Home of all Learning...

Home of all Learning...

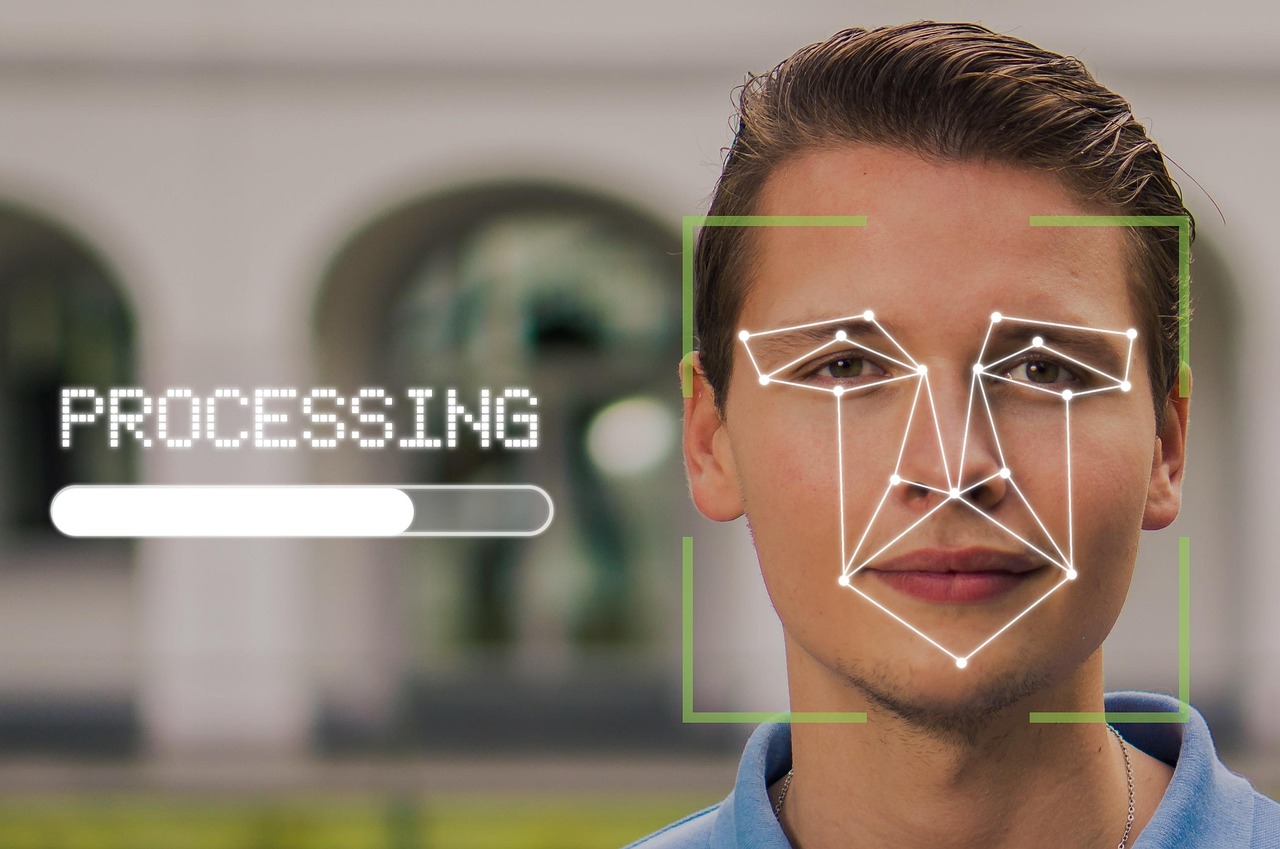
Discover how biometrics improve healthcare by enhancing patient identification, reducing errors, and strengthening data security. Explore real-world examples, benefits, and the future of health biometrics.

The trauma bay was loud, bright, and tense. A middle-aged man arrived unconscious—no wallet, no phone, no family. The triage nurse lifted his index finger to the scanner, and within seconds his full history appeared, including a severe allergy that changed the course of treatment. That quiet “beep” didn’t just unlock data; it protected patient safety and gave the team a head start.
People often ask, Why is biometrics important in healthcare? The short answer is that identity is the foundation of care: if you’re not sure who the patient is, every decision is a gamble. This is the importance of biometrics in healthcare—it reduces guesswork and risk, and it sets a new standard for modern healthcare technology. In plain terms, here’s how biometrics improve healthcare in everyday clinical reality: faster identification, fewer errors, smoother coordination, and more confidence at every touchpoint of care.
You may want to read I Stopped Eating After 6:30PM for 21 Days — Here’s What Happened to My Body and Brain”
At its core, health biometrics uses unique human traits—face, fingerprint, iris, voice, even vein patterns—to recognize a person reliably. When those traits are tied to records, teams can retrieve the right chart, in the right moment, for the right person. Hospitals deploy cameras, scanners, and secure software so that clinicians can verify identity quickly and protect secure patient data without juggling passwords.
You’ll see biometrics examples across the care journey: a face scan at check-in, a palm or iris scan to open restricted doors, and voice recognition to verify a patient on a telehealth call. On the front line, biometric authentication replaces sticky notes and shared logins with something far stronger. In labs and imaging centers, a biometric medical test workflow confirms identity before samples are drawn or scans are taken—tightening the chain of custody and supporting electronic health records (EHRs) that clinicians can trust.
Fingerprint technology remains a workhorse. Many clinics deploy biometric fingerprint stations at registration and in phlebotomy areas, so the identity check moves at the speed of a tap. And when care gets busy, nurses lean on tools and protocols often called biometric nursing—using a scan to chart vitals or unlock medication carts while keeping the clinical workflow moving.
Read Also – Liposuction vs Healthy Diet: Real Weight Loss Results No One’s Showing You Online
Let’s tackle the big question again: Why is biometrics important in healthcare? Because identity errors cascade. A mislabeled sample, a mixed-up prescription, or a chart pulled for the wrong patient can derail treatment and erode patient trust. Biometric tools close those gaps by tying a unique trait to a single longitudinal record.
Fraud is another pressure point. Health systems combat medical identity theft daily, from stolen insurance numbers to falsified visits. When biometric authentication stands between the front desk and the chart, impostors hit a wall, and secure patient data stays protected. The ripple effect is real: fewer billing disputes, fewer duplicate charts, and better hospital efficiency from intake to discharge.
This is also the practical importance of biometrics in healthcare for teams under pressure: with a scan, the right chart opens, orders attach to the right identity, and the care team buys back minutes that can save a limb—or a life.

People also ask, What are the 7 characteristics of biometrics? In healthcare settings, these seven qualities determine whether a modality is useful at scale:
Universality – Everyone has the trait (e.g., fingerprints or face) so nobody is excluded.
Uniqueness – One person’s trait is distinguishable from another’s, crucial for biometric patient identification in healthcare.
Permanence – The trait remains relatively stable over time; records stay consistent.
Collectability – It’s practical to capture in busy clinics and emergency rooms.
Performance – It delivers speed and accuracy without dragging down clinical workflow.
Acceptability – Patients and staff are comfortable using it, which strengthens patient trust.
Circumvention Resistance – It’s extremely difficult to hoax which makes it harder for people to obtain medical identities.
When a technology checks all seven boxes, it’s positioned to lift hospital efficiency and keep the system dependable for frontline teams.
People also ask, What are the benefits of using biometrics? Think in four layers:
Safety: Correct identity means safer meds, safer procedures, and stronger patient safety across units.
Speed: One scan can open electronic health records (EHRs) instantly, trimming delays and improving patient experience.
Security: Better access controls and audit trails make it harder for bad actors to reach secure patient data.
Operations: Fewer duplicates and billing issues translate to clearer data and better healthcare technology ROI.
All of this supports biometric patient identification in healthcare as a backbone for accurate charts, clean orders, and fewer avoidable errors.
Here’s the practical middle ground—how biometrics improve healthcare on a normal day. Registration is the first win: a face or finger scan pulls the right record before the first question is asked. In infusion centers and wards, a quick scan verifies the patient and the medication match. In radiology, a biometric medical test checkpoint confirms identity before the scan, so results never drift into the wrong chart.
Case teams also use biometrics fingerprint checks for bedside medication dispensing and specimen labeling. These steps protect patient experience by cutting rework and explaining less and caring more. Over time, consistent matches and reduced duplicates become powerful biometrics examples that convince even skeptical clinicians that the system is there to help.
Another frequent question is, How can we improve the quality of patient care? Start by eliminating identity doubt. When a scan pulls the right chart, decisions speed up and errors drop. Nurses rely on biometric nursing protocols to document quickly in real time, so handoffs are clean and the story of the admission is clear.
Next, integrate identity with orders. When barcode meds, wristbands, and biometric patient identification in healthcare all align, it’s much harder for mix-ups to sneak through. Tie this to electronic health records (EHRs) and you lift both accuracy and hospital efficiency. The last mile is coaching: teach staff that identity checks are not just a box to tick; they are the quiet backbone of quality that patients can feel.
Security is not just an IT concern—it’s a clinical requirement. With biometric authentication at portals and workstations, fewer passwords float around, fewer accounts get shared, and secure patient data remains contained. Patients who understand the safeguards extend more patient trust, and they’re more candid about sensitive histories that change care.
This is where biometrics examples multiply: a controlled-substance cabinet that opens with a scan; a telemedicine session that verifies the caller’s identity; a lab kiosk that validates who is about to be swabbed. Each step resists medical identity theft and smooths the edges of the day for staff and patients alike.
On the human side, biometrics fingerprint stations anchor check-in, lab draw, and medication workflows. When teams rehearse downtime procedures and educate patients, adoption rises. Small wins—fewer mislabeled specimens, faster chart access—compound into larger ones: clearer documentation, fewer billing edits, steadier clinical workflow.
Meanwhile, biometric nursing isn’t a gadget trend; it’s a mindset. It means relying on a fast, reliable identity signal at the point of care so that fatigue, noise, or shift changes don’t chip away at safety. Over months, the result is quieter nights, fewer callbacks, and a steadier cadence of work that lifts patient experience.
Teams are already asking about the future of biometrics in healthcare. Expect multimodal systems—face plus finger, or palm plus voice—so even if one modality fails, the other succeeds. Wearables will broaden health biometrics beyond the hospital walls, streaming vital signs with consent and plugging insights back into care plans. As models learn, they’ll spot anomalies faster and help staff focus.
In parallel, back-end design will harden against medical identity theft, while front-end touches will stay simple and compassionate. That balance—strong defenses, soft edges—is how the future of biometrics in healthcare becomes daily practice rather than distant promise.
Identity is the first clinical question. Accurate verification protects patient safety, cleans up orders, and protects secure patient data so clinicians can treat with confidence.
They sharpen hospital efficiency and speed access to charts, while reducing fraud and boosting patient trust—all with fewer manual steps for staff.
Start with biometric patient identification in healthcare, reinforce it with medication and specimen checks, and teach teams to use identity signals to streamline clinical workflow.
Universality, uniqueness, permanence, collectability, performance, acceptability, and circumvention resistance—each one helps teams select modalities that fit real-world healthcare technology constraints.
In the end, the best technology disappears into the routine. A scan here, an unlock there—and the right record opens, the right med is given, and the right story is told. This is how biometrics improve healthcare in the moments that matter: fewer identity errors, stronger protections, and care that moves at the patient’s pace. The importance of biometrics in healthcare lives in these small wins that add up to safer halls and calmer shifts. As leaders plan the future of biometrics in healthcare, the goal remains simple—defend the data, speed the work, and deepen patient trust so people feel seen and safe.